Week 2: MRI and Orthopedics Research
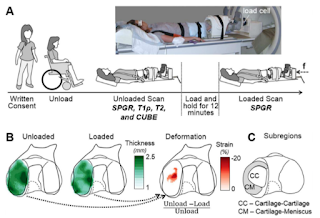
This week I had the opportunity to observe some MRI scans for various research projects. On Monday we performed a unique scan of a patient who had previously received a meniscal graft. The patient's knee joint was loaded to half their body weight using an MRI compatible force plate and imaged to detect localized compression of the tissue. These strain maps may eventually be used to determine whether the graft is effectively distributing loads or if a revision may be necessary. In addition to imaging patients, the MRI lab scans animal tissues which often come from the Cornell University vet school. This often requires special preparation to enable the use of certain coils and protect both the scanner an sample. Last week were able to scan a horse hoof using ultrashort echo time (UTE) imaging techniques (see Week 1 blog post). This week I studied different methods to quantify T2 relaxation times in tendon using these images. On Thursday we attempted to scan rat patellar tendons tha...









